A UTD chemist graduate is engineering a simpler and safer way to inject powder vaccines painlessly, potentially revolutionizing the healthcare industry.
Ph.D. student Yalini Wijesundara created the Metal-Organic Framework Jet, which can administer therapeutic agents through the skin with just a puff of compressed air. The technology could be applied in veterinary medicine, agriculture, vaccinations and cancer treatment.
Debuting among 10,000 presentations at the spring summit of the American Chemical Society in late March, Wijesundara presented the MOF Jet injector as a relatively painless to administer vaccines, which could simplify the vaccination process and remove the pain and hygiene concerns of the traditional needle injection.
“It’s just like a feeling of being hit with the NERF gun, like a puff of air,” Wijesundara said. “[A] considerable amount of people don’t like to get vaccinated because they have this needle phobia and they stress about it.”
An effective alternative to liquid vaccines, powder vaccines don’t require refrigeration at below 46 degrees Fahrenheit, making them cheaper and easier to transport. Not only could it save companies money, but it makes vaccines more accessible and affordable by addressing the thermal challenges of vaccine delivery to remote areas. Pharmaceutical companies have considered inhalers or pills, but UTD is one of the first research institutes to recently show evidence that jet injectors are the future of vaccines.
The original investigator, Jeremiah Gassensmith, associate professor of chemistry and biochemistry at UTD, constructed a homemade gene gun otherwise known as a biological ballistic particle delivery system. Gassensmith built the gene gun during pandemic boredom for about $150 as opposed to the most popular commercial gene gun system at about $30,000; this would become the foundation for the MOF-Jet. Gassensmith suggests that not only will the MOF Jet be safer, but in time, it will be simpler to use for both medical professionals and patients. Currently, needlestick biohazards are responsible for the transmission of nearly 60 infectious diseases, including hepatitis and HIV, and an estimated 11 million unsafe injections occur internationally every year.
“[Needles are] an effective way, but an unfortunate way, to spread communicable diseases in clinics,” Gassensmith said. “And wherever you have any need for needle sticks, you have some need for somebody to be trained with it. The idea behind [MOF-Jets] is to get rid of that.”
While the MOF-Jet is a promising innovation, it’s not the first time jet injector technology has been used. During the 1960s, they were used for mass vaccination efforts to prevent smallpox and were especially popular with armed forces due to the fast and tireless procedure. However, the World Health Organization has since rejected the use of jet injectors internationally due to a list of concerns including cross-contamination, splashback, retrograde flow and the spread of hepatitis B. The MOF-Jet eliminates that problem almost entirely by replacing pressurized liquid with compressed air.
Gassensmith and Wijesundara said these powder vaccines will be restrained in a MOF matrix that prevents them from interacting or breaking down up to 572 degrees Fahrenheit. Once ready for injection, the vaccine will be delivered with a puff of compressed air at a certain velocity to be microscopically delivered into the skin to begin an immunology process without allowing blood to escape. Not only does the MOF-Jet distribute therapeutic agents more evenly, but it also uses Wijesundara’s discovery on how different carrier gasses in the injector can affect the timeframe of these releases.
Wijesundara discovered the type of air used, whether standard gas or carbon dioxide, affects the pH levels that allows cells in the MOF matrix to dissolve and release the vaccine. The pH levels only begin to impact the MOF matrix when introduced to the water inside the skin, which with carbon dioxide, increases acidity for swifter administration. This means not only can the MOF-Jet administer therapeutic agency over time, but also immediately during emergencies.
Testing is currently being done on agriculture, proving that the MOF-Jet allows for gene exposure in vegetation. It’s in the phases of preliminary studies, but Wijesundara expressed how this could affect insulin and cancer treatment. Insulin cannot survive at room temperature, but by putting it in a solid formulation like powder and using a MOF-Jet, it can have an extended shelf life that’s more accessible. For cancer treatment, the MOF-Jet can bombard skin tumors in a more widespread and effective method, treating the entire tumor rather than injecting parts of the tumor, which can lead to bleeding afterward.
“There is a long way to go to clinical level,” Wijesundara said. “This is a system we can deliver [and] we can recreate in a patient convenient way, but this is the basic idea. We can put this into society so they can develop, spend some more money on it, and make it more convenient, more mobile.”
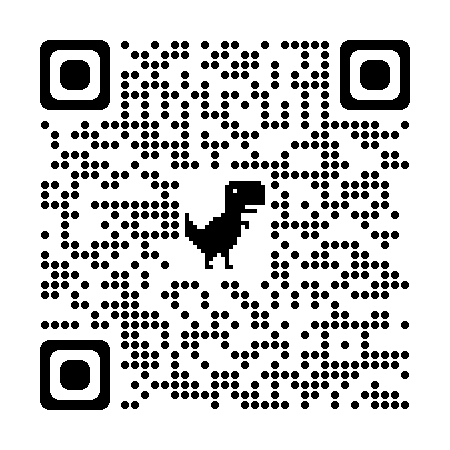
Wijesundara’s latest research can be read here. (Online)
A link to Wijesundara’s research can be found on our website. (print)
Her QR is below:
Leave a Reply